- Detailed rules on new foundation trust, IHO and neighbourhood provision to be developed this summer
- Aspiring IHOs will be tested on local relationships, to avoid “turf wars and land grabs”
- Private funding for hospitals not in the plan, but NHS CEO says Treasury’s objections can be overcome
- Replacement for block contracts “must support neighbourhood care”
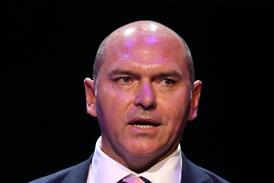
Sir Jim Mackey expects several of the NHS’s first “integrated health organisations” to be created next year.
Today’s 10-Year Health Plan says the best performing foundation trusts will be allowed to evolve into IHOs which will be given a capitated budget to run a wide range of range of acute, community and primary care services for their population, as revealed by HSJ last month. The plan compares them to the US accountable care organisation model.
Sir Jim also told HSJ that:
- Many of the proposals put forward in the 10-Year Health Plan would be driven by detailed strategies developed “before winter”
- The debate on how far the NHS should move away from block contracts was still ongoing
- Deficit funding will effectively be phased out from next year using a new “pace of change” policy – while Wes Streeting last week said ”the fund will not go to trusts which run deficits this year”
- The Treasury remain unconvinced about allowing private lenders to provide NHS capital funding for hospitals.
The NHS chief executive said he expected the “few” first IHOs to be created next year. He added: “There are a few out [FTs already out] of the blocks, a few to be determined. But [judging by] the people who send me a text or [have a] phone call, there’s going to be a lot of people sitting at the doorstep, with their applications ready.”
The plan itself goes further than previous drafts to say IHOs will “over time… become the norm” – rather than coexisting with other models in different areas.
Sir Jim continued: “One of the [tests] for us will be, ‘how strong are the relationships here?’ We’re expecting clinical teams to work together with councils, with the voluntary sector, with housing providers, to bring neighbourhood care. They’ve got to have the relationships to do that and the capability to actually work with others.
“We won’t allow ourselves to descend into the power, land-grab thing of the past where it’s all about the person dominating the system.”
Sir Jim said he would be clear with trust leaders that “if anybody thinks this is about me taking over absolutely everything in my place”, they would have to prove partners supported that idea. However, he stressed this did not mean particular organisations having a “veto” on IHOs being created.
He said detailed frameworks for IHOs, the “new FT” regime, or commissioning of neighbourhood health would not be published immediately.
The Plan was, he argued, about creating “energy and enthusiasm” and would be followed by detailed proposals developed with local leaders over the summer, and published before winter.
The NHSE CEO said planning guidance and allocations for 2026-27 would be published in October, and added: “We need to get quite a lot of this in place before we’re in the full battle of winter [when] it’s always very hard for people to be thinking about the future and developmental stuff.”
Sir Jim said local leaders were “hungry to see what we’re going to do next” and said he wanted the centre to get “a bit breathless” in trying to ”keep the pace going, the rate at which we can produce the rules, and get to the next step”.
Funding systems
The 10-Year Health Plan says there will be a move away from block contracts – which currently fund huge amounts of non-elective hospital care – in 2026-27. It promises both a shift towards a more tariff-style regime, as well as incentives linked to patient experience and moving care into the community. The plan also says “year of care” payments – incorporating a range of services including general practice – will be trialled.
Last week, HSJ revealed proposals for a payment system for emergency care which would base payments on a mixture of block allocations, waiting times, and shifting towards “neighbourhood health”.
Asked what would replace block payments next year, Sir Jim said: “There’s pretty strong unanimity that block is the wrong thing, but there are different views on whether you [instead] go full volume-related [tariff] or some kind of [hybrid system combining activity and other measures].”
Meanwhile, the Plan reveals that as well as reviewing the GP funding formula, there will also be a review of the integrated care board allocation formulas, which distribute about £150bn this year.
Sir Jim said the independent allocation committee would rapidly “kick the tires on the formula” this summer, as there is “a feeling about do we need to go further on deprivation?”.
Both the Plan and Sir Jim struck a different note on deficit support for trusts than that made by Wes Streeting last month who said: “Thanks to the reforms we have made to bear down on wasteful spending, the fund will not go to trusts which run deficits this year.”
The Plan says deficit support, this year worth £2.2bn, would only begin to be withdrawn next year, and Sir Jim said likely changes to the formula, and a “pace of change” policy, would mean it is not removed immediately. At present, several systems with high deprivation – such as Lancashire, Greater Manchester, Cheshire and Merseyside, and South East London – are big recipients.
The NHS CEO said: “In reality if you’re currently a place that receives a big chunk of money for deficit support, when that goes back into the sausage machine and gets played out on the formula, and maybe with a bit more emphasis on deprivation, you’ll get some of it back for legitimate reasons – not just the fact that you’re spending somebody else’s money…
“No one expects everything to get perfect overnight. We’re moving a lot of things at the same time, both in allocative processes but also in more practical and operational processes… So, nobody [wants us to move] so quickly everything breaks [or] grinds to a halt. But we can’t just keep ignoring the fact that parts of the country are spending money that… should be spent somewhere else.”
Private finance
Sir Jim said he still hoped major hospital builds could be funded with private finance in coming years, despite Treasury reservations blocking the inclusion of this in the 10YHP.
The NHS CEO said: “What most people wanted to see was, ‘can we do this again for big hospital infrastructure?’ And that’s not just people who are running hospitals, it’s the lenders, the pension firms, the construction industry. They’re all kicking doors down…
“We haven’t been able to persuade Treasury that this is something we can absolutely go hell for leather at just yet. But they have been helpful in describing what their anxieties are, in the process, and we now know.”
He said the Treasury had “been quite clear they will take a lot of convincing”, but added: “I’ve talked to people out there in trusts who can meet… tests [such as] not repeating the problems of the past, not just creating long-term liabilities that are more expensive, but genuinely bringing in innovation [and] new approaches…
“The plan is silent because we haven’t got agreement from Treasury on it… But I know from conversations with colleagues there’s a confidence that those tests can be met.”
Although there is no clear backing for using private finance for capital projects in the plan, it does say it will be explored and trialled for particular projects.
Sir Jim said he thought it would be used soon for multiple community developments, and there would now be “more permissive” approvals for NHS “commercial” development proposals, such as those based on developing housing for staff or other “revenue streams”.
In his time as chief executive of Northumbria Healthcare FT, Sir Jim managed to re-finance the trust’s PFI via a borrowing agreement with the local authority.
Amended at 4.40pm on 3 July to clarify what Sir Jim meant on two points.
Exclusive: 10-Year Plan published without delivery chapter
- 1
- 2
- 3
- 4
Currently reading
Mackey: Multiple ACO-style providers to be ‘created next year’



























9 Readers' comments